Breast eczema is a condition that affects the skin on or around the breast and may affect over 500,000 people each year. Even with all of these dermatitis diagnoses, the condition is not really talked about.
The lack of information on symptoms, causes, and treatment options is frustrating! If this sounds like your situation, then this is the article you have been looking for.
As an Amazon Associate, I may receive compensation for qualifying purchases.
What is breast eczema?
Breast eczema, also known as nipple eczema or areola eczema, is a type of skin inflammation that affects the breast area. It is a common condition that can occur in both men and women, but it is more commonly found in women.
What does breast eczema look like?
Breast eczema can look slightly different for everyone. The most common presentation is redness, dry patches, and itchy skin. In some cases, the skin may appear leathery or thickened. Breast eczema can affect one or both breasts and may spread to the surrounding skin.

This image is not your typical picture of breast eczema and is considered a severe case. This picture is from a breastfeeding woman who has developed weeping eczema of the nipple and areola and has also developed a staph infection.
It is important to consult a healthcare provider for an accurate diagnosis and treatment plan if you experience any of these symptoms.
Eczema on the Breast vs Psoriasis
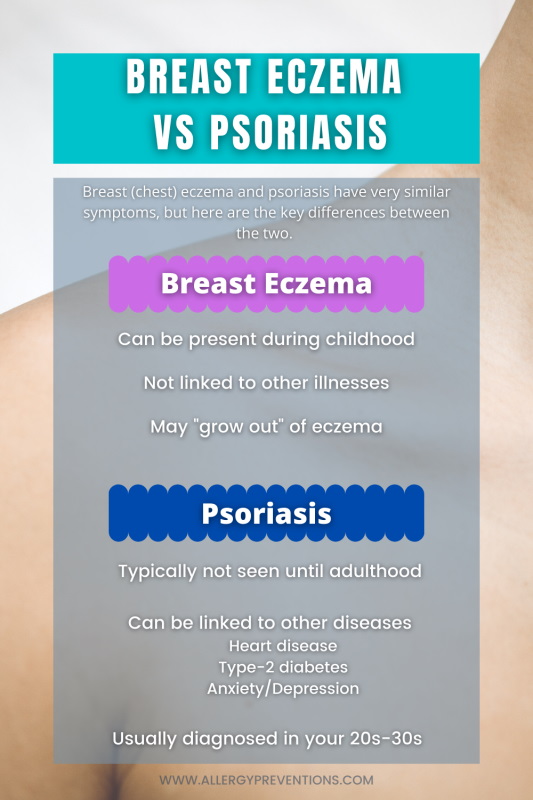
Both of these conditions give similar symptoms which can make it challenging to know which condition you may be experiencing.
Psoriasis.org explains that psoriasis is a chronic immune system disease that can lead to other conditions like heart disease, type-2 diabetes, anxiety, and depression. Such links are not associated with eczema or dermatitis.
Additionally, psoriasis is not usually seen until the ages of 20 to 30 years old, and not typically during childhood. Eczema including on the chest can be present during childhood and carry into adulthood, or the child may “grow out” of eczema altogether.
Paget’s Disease vs Breast Eczema
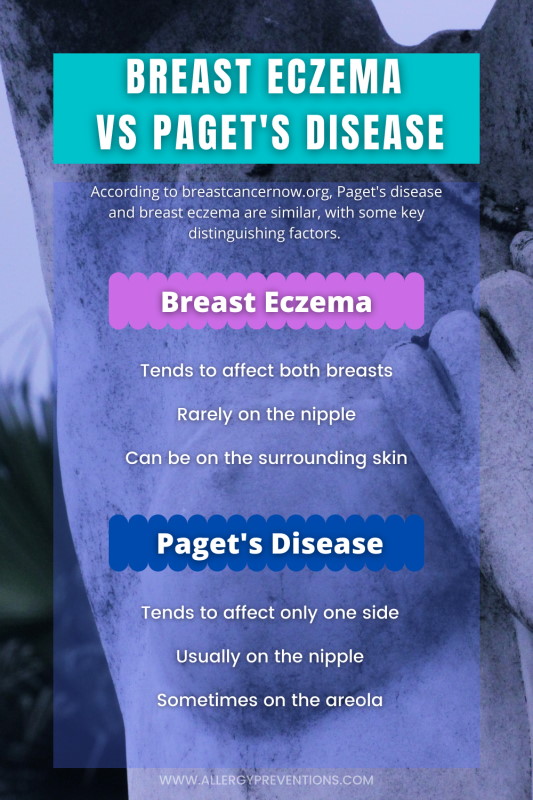
According to breastcancernow.org, Paget’s disease is an (uncommon) breast cancer that occurs in less than 5% of women with breast cancer. Paget’s disease can cause red and scaly rash-like symptoms on the nipple. Sometimes the rash does spread to the areola (dark skin around the nipple).
Paget’s Disease
- Tends to affect only one side
- Usually on the nipple
- Sometimes on the areola
Breast Eczema
- Tends to affect both breasts
- Rarely on the nipple
- Can also be on the surrounding skin and/or chest
How common is breast eczema?
Fairly common. Potentially 500,000 people are affected by breast eczema in the United States. According to the NEA, eczema as a whole affects over 31 million people in the U.S. The most popular places to get eczema are the joint areas (wrists, knees, elbow), face, neck, and legs.
Assuming the most popular regions where eczema develops on the body take up 90% of the cases, that leaves 10% (3.1 Million) cases for less common areas like the ears, back, chest, feet, lips, etc. From my research, and reading about breast eczema stories, I believe breast eczema affects around half a million people.
Is eczema on the breasts serious?
Not typically, but it can lead to more serious conditions. In extreme cases, breast eczema can lead to inflammation and swelling that may affect your overall comfort, especially with tight-fitting clothes. Additionally, the potentially dry and cracked skin from eczema may increase your chances of developing a skin infection.
Who does breast eczema affect?
Eczema on the breast or chest can affect anyone. According to the Cleveland Clinic, you have an increased risk of developing breast eczema if you meet one or more of the following factors.
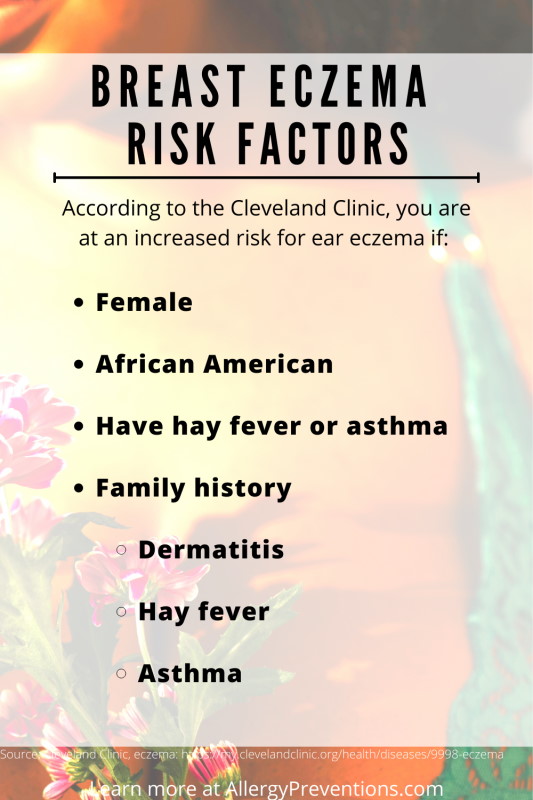
Risk Factors
- Female
- African American
- Suffer from hay fever and/or asthma
- Family history
- Dermatitis
- Hay fever
- Asthma
Symptoms of Breast Eczema
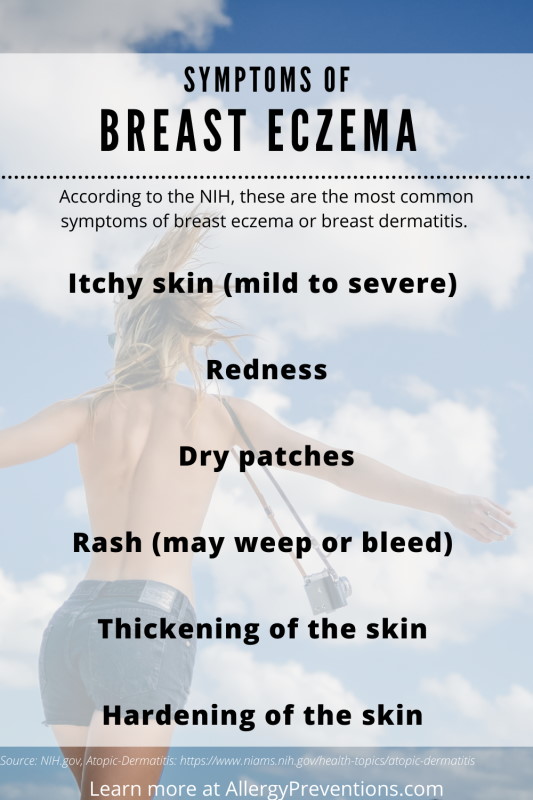
The most common symptom of breast eczema is itchy skin on or around the breasts, which can range from mild to severe. According to the NIH, additional symptoms may include the following:
Signs and Symptoms
- Itchy skin (mild to severe)
- Redness
- Dry patches
- Rash (may weep or bleed)
- Thickening of the skin
- Hardening of the skin
Types of Breast Eczema
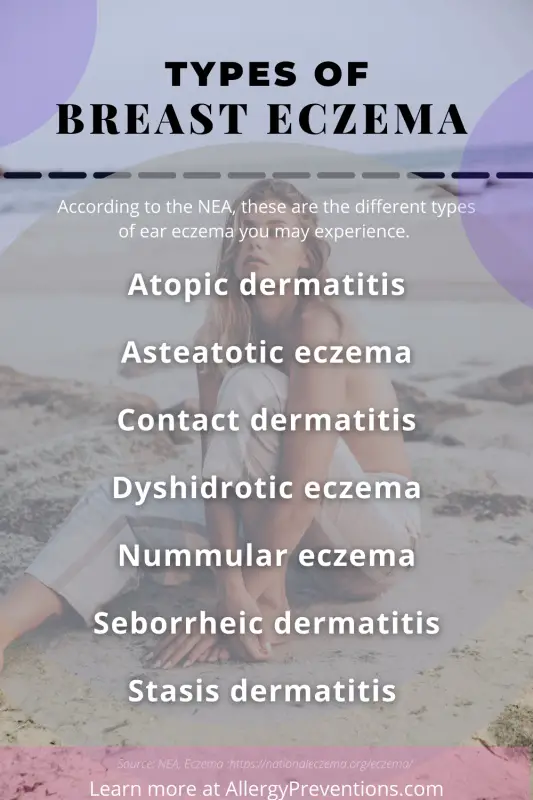
Breast eczema can be caused by many different inflammatory skin conditions. The National Eczema Association explains that there are 7 different types of eczema you can develop on your breasts.
- Atopic dermatitis
- Eczema from genetics
- Asteatotic eczema
- Dry skin from moisture loss
- Contact dermatitis
- Inflammation from touching something
- Dyshidrotic eczema
- Small blisters appear
- Nummular eczema
- Round patches that look like coins
- Seborrheic dermatitis
- Sebaceous gland inflammation
- Stasis dermatitis
- Poor fluid circulation
Causes
There are many reasons that you may be suffering from breast eczema. Here are the more common causes of flare-ups that have been provided by the NEA.
Potential Breast Eczema Triggers
- Exposure to dry air (low humidity)
- Extremely hot or cold environments
- Soap/body wash
- Shampoo
- Bubble bath
- Face wash
- Laundry detergent
- Fabric softener
- Wool and polyester
- Cleaners/disinfectants
- Natural liquids on the skin (fruits, vegetables, and meats)
- Candle fragrance
- Metals (usually nickel)
- Formaldehyde (additive in some disinfectants, vaccines, glues, etc.)
- Isothiazolinone (make-up removers, baby wipes)
- Cocamidopropyl betaine (soap, lotion, shampoo, thickener)
- Paraphenylenediamine (leather dyes and temporary tattoos)
As you can see, there are so many triggers, and this isn’t all of them. Additionally, the cause may be from your genetics, or idiopathic (unknown reason). I recommend that you take note of when your notice an eczema flare-up and try to figure out what is causing your symptoms.
Treatments
Home Remedies
Home remedies are usually the first and best place to start for any ailment including breast eczema. These options incorporate items you may have in your home already or are available over the counter.
Bath or Shower
Taking a bath or shower in lukewarm water (not hot) can help replenish some of the moisture in your skin. Ensure you follow these tips to help calm your skin during and after a shower.
- Avoid hot showers
- Limit bath time to 10 minutes
- Pat dry your skin with a towel
- Immediately apply an unscented moisturizer
Use Moisturizers
When you are suffering from an eczema flare-up, the skin is usually dry and mad. Calming the skin and getting it the moisture it needs is crucial for breast eczema treatment. During my moisturizer research, I learned really quickly that there is no one size fits all. Here is a quick rundown of moisturizers.
Lotion
Mostly water-based and doesn’t last very long when moisturizing skin. Good for maintaining moisture in your skin but not the best for repairing or calming it.
An ointment is typically made of oil-based ingredients. The main ingredients you will find are petroleum jelly and sometimes mineral oil. Both of these oils are a beast at protecting and sealing in moisture. Ointments are thick and goopy. This might be what you are looking for if you have a breast eczema flare-up.
Ointment
Moisturizing Cream
Creams are the middleman between ointments and lotions. They have a bit of oil like an ointment and a bit of water like a lotion. Moisturizing creams are great for locking in moisture without the heaviness and greasiness of an ointment.
Antihistamines
Eczema is usually related to allergies, so using an antihistamine may help relieve some of the itchy and swollen ears. There are many over-the-counter antihistamines these days, so ensure you do your research and have a conversation with your doctor.
Pain Reliever
Breast eczema can cause damaged, dry, cracked skin which can be painful. Your medical provider may instruct you to take a pain reliever or NSAID to reduce pain and inflammation.
Hydrocortisone
Hydrocortisone is a topical steroid that soothes the skin and stops itching. Those of us who are not new to eczema, seem to always have hydrocortisone on hand. You can pick some up on Amazon.com.
Additional Treatment Options
The fact is there is no cure for eczema (NEA). The medical community is consistently working on finding solutions to treat eczema, so your options should expand in the years to come. For now, here are the typical treatments that you can talk about with your doctor for implementation.
Prescription Medications
Sometimes the use of over-the-counter medications or home remedies just doesn’t cut it, your doctor may want to prescribe a medication to get you some relief. Here are the types of prescriptions your Provider may wish to discuss with you.
- Topical Creams
- Injections to calm the immune system
- Oral medications
- UV Light Treatment
Natural treatments
Natural treatments haven’t been well documented for their efficacy but there are many sufferers who swear by these homeopathic approaches. If you are looking to venture into these treatment options, please choose high-quality ingredients and discuss them with your doctor first.
Natural Moisturizers
A big problem with eczema is keeping the skin happy and moist, so you may want to try using a natural moisturizer. The top natural moisturizers that eczema sufferers use are coconut oil and sunflower oil. Of course, if you have a coconut allergy or sunflower allergy, avoid the oils!
Vitamins
Ensuring your body has the proper nutrients to produce healthy skin (and immune system) may help relieve some symptoms. You can look for foods that are rich in these specific vitamins, or find the most natural supplement at your favorite health food store. Here are the supplements studied in the National Library of Medicine Medical Journal.
Probiotics
- Healthy bacteria
- Boosts immunity
- Found in certain foods, or in supplement form
Prebiotics
- Healthy gut bacteria food
- Boosts overall health
- Found in certain foods, or in supplement form
Vitamin D
Vitamin D may play a role in helping chronic inflammation (like eczema), but there simply have not been enough studies to prove or disprove it at this time.
Fish Oil
Fish oil may help with treating eczema, but is not “routinely recommended”. in this journey study, they did note that fish oil “Significantly improved the effects on daily living as compared to placebo”.
Evening Primrose and Borage Seed Oils
Both of these oils came up in 27 studies to find out if they are a good option to treat eczema. The results from the majority of the studies showed some improvement but are not studied enough to be considered an eczema treatment.
The overall results of vitamins as a treatment are not great. This is due to the fact that there just have not been enough quality studies conducted. This does not mean that none of these vitamins will give you relief, just something to consider. Please keep in mind that I am basing this on limited scientific studies. Real users may have experienced better outcomes.
Diagnosis and tests
Discover the different diagnosis techniques and possible tests that may be used to figure out if you do have breast eczema. Breast eczema can look like many other health conditions, so it is important to be evaluated by your doctor.
How is breast eczema diagnosed?
A medical professional will be the one to officially diagnose you with eczema of the breasts. Your medical provider will diagnose based on the clinical findings (what it looks like), and by asking you some standard questions. The questions your doctor may ask are:
- How long has this been going on?
- Any history of asthma, allergies, or hay fever?
- Does anyone in your family have eczema?
- What are your symptoms?
- What makes your symptoms better or worse?
Be prepared to answer the above questions, and write down any questions you may have for your doctor.
What tests will be done to diagnose breast eczema?
Your doctor may (or may not) conduct any tests to diagnose breast eczema. If your doctor does believe tests should be accomplished to rule out other conditions, they may conduct an allergy skin test, blood test, or skin biopsy. Usually, your doctor can diagnose during the exam and health history appointment.
Is there a cure?
There is no cure for breast eczema. Eczema or dermatitis is an inflammation of the skin, caused by some other condition (immune system disorders, allergies, environmental exposures, etc.) Finding the root cause of eczema will help you better understand your condition.
Breast Eczema Prognosis
Although breast eczema may be a chronic condition, as long as you are aware of your triggers, know what makes your symptoms manageable, and avoid infections, the outlook of breast dermatitis is good.
Complications
There are some complications with breast eczema that you should be aware of. Complications can be weeping and infection. If you do suspect these complications, please go see your doctor.
Weeping
When symptoms start to get severe you may notice weeping. Weeping is when there is a fluid discharge coming out of the area where you are experiencing eczema. This is your body letting you know that something is up and needs to be evaluated by a medical professional. Untreated weeping or bleeding could lead to infection.
Infection
Infected eczema happens when you develop a skin infection from dermatitis. Below are some of the more common signs and symptoms that your breast dermatitis may be infected.
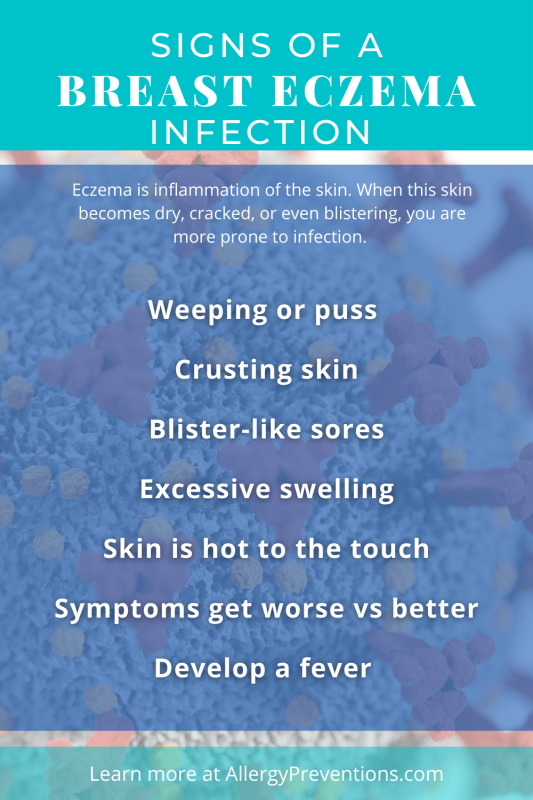
Signs of infection
- Weeping or puss
- Crusting skin
- Blister-like sores
- Excessive swelling
- Skin is hot to the touch
- Symptoms get worse vs better
- Develop a fever
Infections are something that needs to be treated, seek medical assistance right away. Keep in mind this is not an all-inclusive list and you may experience different symptoms. When in doubt, see a medical professional.
Prevention
Preventing symptoms or flare-ups is a great approach when managing breast eczema. The first step in preventing eczema is to know your triggers and avoid those triggers if possible. If not, there are still some things you can do to hopefully make life a bit easier.
Switch Household Products
At our home, we use the EWG to research all of our products. The EWG is a website (they have an app too) that tells you how good or bad for you your household products are. We ended up switching all of our soaps, body washes, and laundry detergent for something healthier. The EWG made it so easy to research.
Use the EWG and look up your specific products. How do they rate?
EWG Items to Investigate
- Shampoo
- Body wash
- Handsoap
- Laundry detergent
- Face wash
- Cosmetics
- Lotion
- Sunscreen
- Household cleaners
Apply moisturizer
Unfortunately with breast dermatitis, you are going to have a daily battle with your skin. Your goal will be to keep that skin healthy, moisturized, and not mad.
FAQ
Here are the frequently asked questions about breast eczema, from actual readers like you!
Can I put steroid cream on my breasts?
Yes. steroid cream is “external use” but consult a doctor first, especially if breastfeeding.
Does coconut oil cure breast eczema?
No, there is no cure for eczema. But, coconut oil may help relieve itchy skin caused by eczema.
Is it possible to have eczema on your breast?
Yes, you can get eczema on and around your breasts. Eczema is a skin inflammation that can show up anywhere on the body.
Is aloe vera good for breast eczema?
Yes. Aloe vera is good for calming skin affected by eczema.
How do I get rid of eczema on my breasts?
Knowing the cause of eczema will be needed to get rid of eczema on your breasts. For example, if you discover that your body wash is causing eczema, switching to a different body wash should get rid of your dermatitis.
Can I put Cortisone 10 on my breasts?
Yes. Cortisone (Cortizone 10) states for external use only. Always read the instructions and consult your doctor.
Why is my eczema oozing or weeping liquid?
Potentially from an infection. If your eczema is oozing or weeping, you may have an infection and should seek medical attention.
Is breast eczema contagious?
No. breast eczema is not contagious.
Will petroleum jelly help breast eczema?
Yes. Petroleum jelly can help relieve breast eczema symptoms, and create a moisture barrier for the skin.
Can breast eczema be cured?
No. There is no cure for breast eczema, but the symptoms can resolve.
How does breast eczema affect my body?
Breast eczema can affect your body in a number of ways including itchiness, dryness, irritation, and hardening of the skin.
Final Thoughts
So, that is breast eczema in a (really big) nutshell. Was there something I missed or that you would like to see more information on? Send me an email and I will get researching! chris@allergypreventions.com
