Eczema, commonly known as dermatitis, is a chronic skin condition that affects millions. It is characterized by red, itchy, and inflamed skin, which can be painful and frustrating to deal with. Eczema can affect people of all ages, but it is most common in children. In this article, we will provide you with a deeper understanding of symptoms, diagnosis, and treatment options, to help you better manage this condition effectively.

When you buy something through one of the links on our site, we may earn an affiliate commission.
Table of Contents
What is Eczema?
Eczema is a long-lasting skin condition that tends to make your skin red, and itchy, and might even cause a rash or bumps. It’s something that can happen to anyone, from babies to grown-ups. But don’t worry, you can’t catch it like you can catch a cold from someone else.
Types of Eczema
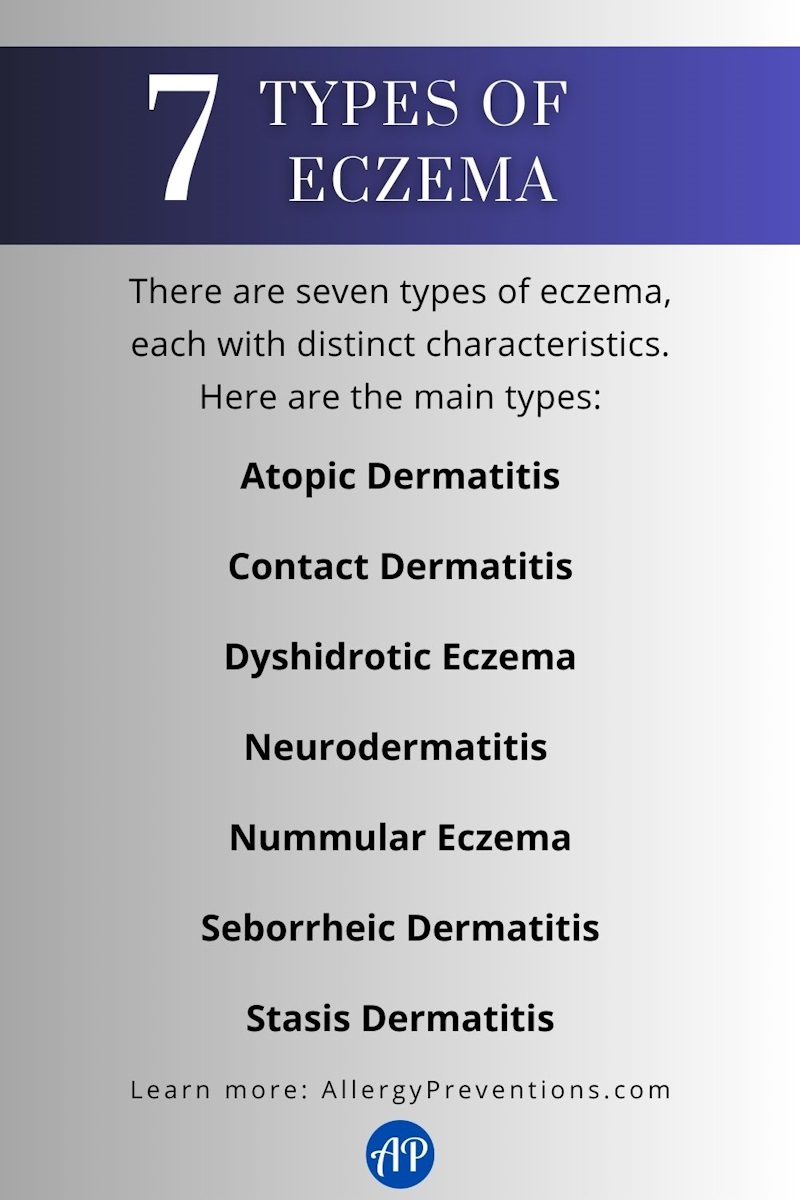
Eczema, also known as dermatitis, refers to a group of skin conditions that cause inflammation, itching, and irritation. There are several types of eczema, each with distinct characteristics. Here are some common types:
- Atopic Dermatitis: This is the most common type of dermatitis, often associated with allergies and a family history of allergic conditions like asthma or hay fever.
- Contact Dermatitis: Can be “allergic” or “irritant”, depending on what substance your skin comes in contact with.
- Dyshidrotic Eczema: Causes small, itchy blisters to develop on the hands and feet, often accompanied by intense itching.
- Neurodermatitis (Lichen Simplex Chronicus): Characterized by thick, scaly patches of skin caused by repetitive scratching or rubbing.
- Nummular Eczema (Discoid Dermatitis): Characterized by round, coin-shaped patches of inflamed skin that are often very itchy.
- Seborrheic Dermatitis: Commonly known as dandruff when it affects the scalp, seborrheic dermatitis causes red, scaly patches and flaking.
- Stasis Dermatitis: Also known as venous eczema, this type occurs in the lower legs due to poor circulation and fluid buildup.
Keep in mind, that this list is of the main types of eczema. There are many other subsets or variants of dermatitis; for example lichenoid eczema, asteatotic eczema, and spongiotic dermatitis.
Is eczema the same as dermatitis?
Eczema and dermatitis are terms that are used interchangeably but mean slightly different things. Dr. Jeremy Fenton explains that dermatitis is a general term that refers to inflammation of the skin. Eczema is a specific skin condition that causes inflammation and can be considered a form of dermatitis.
Where You Can Get Eczema On Your Body
Eczema can appear anywhere on your body where skin is present. Here is a list of the most common places where people often get eczema:
- Ankles and Feet: The ankles and the tops of the feet can be prone
- Back: The upper back is the most common location for eczema on the back.
- Behind the Ears: This can occur behind the ears, leading to redness and itching.
- Chest and Breasts: Can affect the skin on the chest and breasts.
- Face: On the cheeks, around the eyes, and on the forehead.
- Groin Area: The groin area, including the inner thighs, scrotum, and penis.
- Inner Elbows: The creases on the inner side of the elbows are a common location.
- Knees: The top of the knee, and creases on the back side of the knees are also often affected.
- Neck: The neck area, especially the back of the neck, can be the most prone.
- Scalp: Causing flakes, itching, and redness.
- Wrists and Hands: Appearing on the wrists, hands, and fingers.
These are just some of the common areas where dermatitis can occur. It’s important to note that skin conditions can vary from person to person, so it might appear in different places for different individuals.
Common Eczema Symptoms
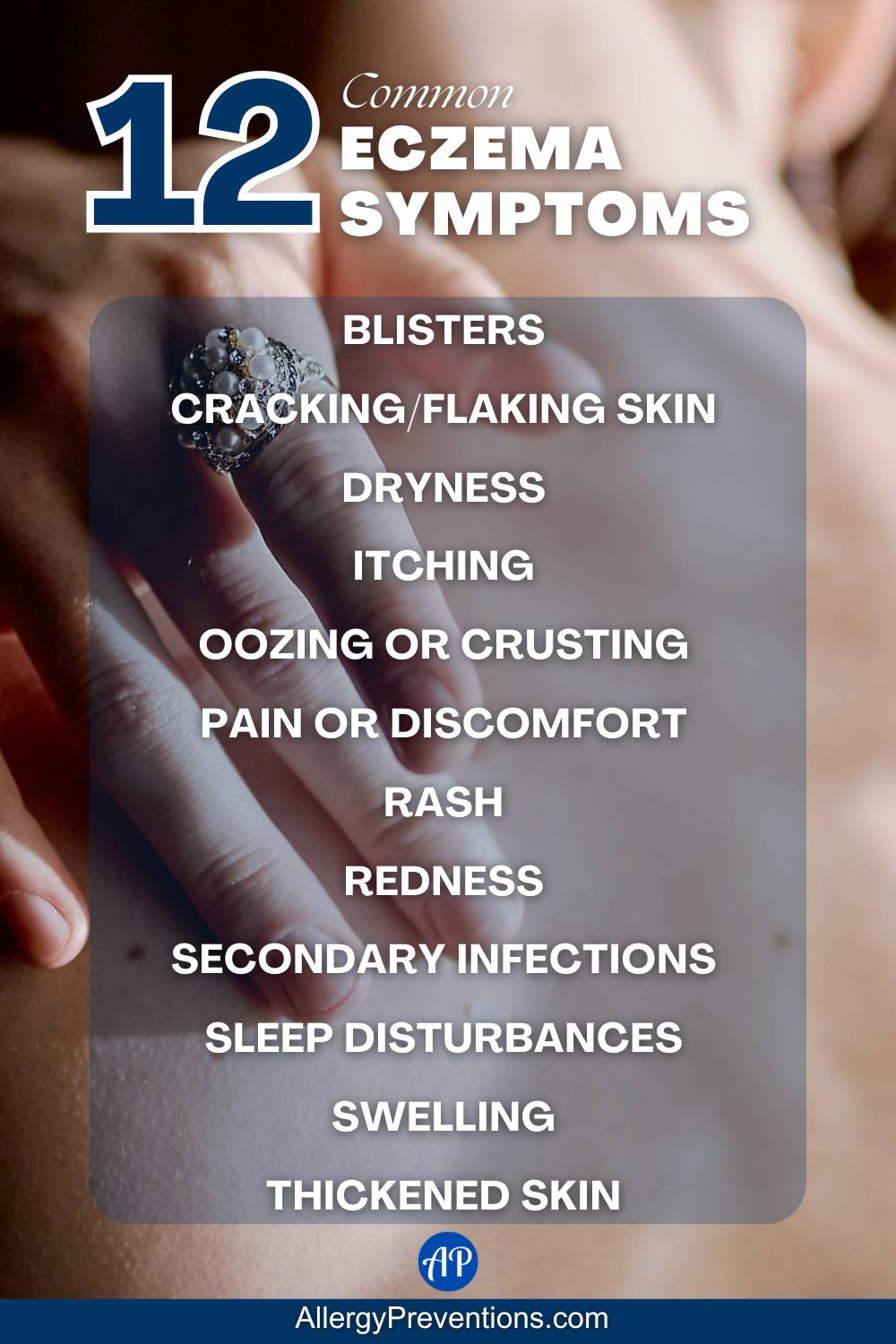
The symptoms of eczema can vary based on the specific type and severity of the condition. Here are some common symptoms associated with eczema:
- Blisters: Small, fluid-filled blisters can develop on the palms, fingers, soles of the feet, or toes.
- Cracking and Flaking: The skin may crack and peel, especially in cases of severe dryness. Flaking may be more noticeable in certain types of eczema such as seborrheic dermatitis.
- Dryness: The skin tends to be dry and may feel rough to the touch. The skin’s natural barrier function is compromised, leading to increased moisture loss.
- Itching (Pruritus): Intense itching is one of the hallmark symptoms. Itching can be mild to severe and is often the most bothersome aspect of the condition.
- Oozing and Crusting: Dermatitis patches can become moist, leading to oozing and the formation of crusts. Scratching can exacerbate this symptom.
- Pain or Discomfort: In severe cases, patches of skin can become painful, especially if they become infected due to scratching or other irritations.
- Rash: Eczema can cause red, raised patches or a rash on the skin. These patches may be accompanied by small bumps, blisters, or areas of oozing and crusting.
- Redness (Erythema): Affected skin areas may become red or inflamed due to increased blood flow and inflammation in response to irritants or allergens.
- Secondary Infections: Scratching can break the skin barrier, making it more susceptible to bacterial, viral, or fungal infections.
- Sleep Disturbances: Intense itching can interfere with sleep, leading to sleep disturbances and decreased quality.
- Swelling: Inflamed skin can become swollen, making affected areas appear puffy or thicker than usual.
- Thickened Skin: Over time, repeated scratching or rubbing can cause the skin to become thickened and leathery, a condition known as lichenification.
It’s important to note that eczema symptoms can come and go, this is called a flare-up. The triggers and severity of these symptoms can vary widely among individuals. If you suspect you have eczema, it’s advisable to consult a dermatologist for proper diagnosis and treatment.
Root Causes of Eczema
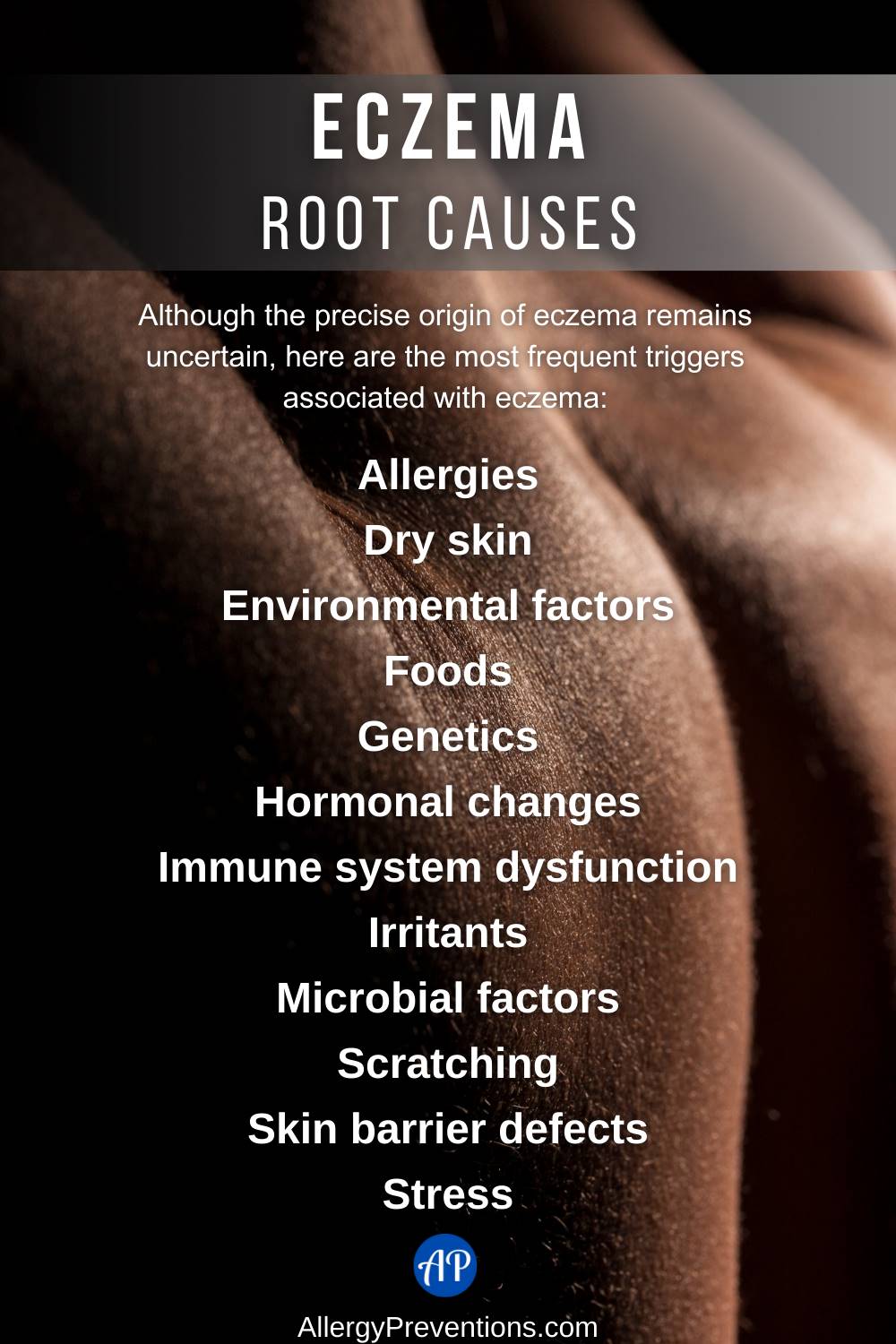
The exact root cause of eczema is unknown, but it is believed to be caused by a combination of genetic and environmental factors. Here is a list of the most common eczema-causing triggers:
- Allergies: Allergic reactions to substances such as pollen, pet dander, certain foods, or dust mites can exacerbate eczema symptoms or trigger flare-ups in susceptible individuals.
- Dry Skin: When the skin loses moisture and becomes excessively dry, it can become more prone to eczema-related inflammation. Dry skin is often a trigger for flare-ups.
- Environmental Factors: Cold, dry weather can worsen symptoms, as can exposure to sudden temperature changes or high humidity.
- Foods: Although rare, certain foods can trigger symptoms in some individuals, especially young children or those with food allergies. Common triggers include dairy products, eggs, nuts, and acidic foods.
- Genetics: A family history of eczema, allergies, asthma, or hay fever can increase the likelihood of developing eczema. This suggests a genetic predisposition to the condition.
- Hormonal Changes: Hormonal fluctuations, such as those that occur during pregnancy or menstruation, can impact symptoms in some people.
- Immune System Dysfunction: Eczema is often linked to an overactive immune response that leads to inflammation and irritation of the skin. This immune system dysfunction can cause the skin to react more strongly to certain triggers.
- Irritants: Exposure to irritants like harsh soaps, detergents, chemicals, and even some fabrics can lead to flare-ups, particularly in people with sensitive skin.
- Microbial Factors: Certain microbes, such as Staphylococcus aureus bacteria, can colonize the skin of people with eczema and contribute to inflammation.
- Scratching: Persistent scratching can damage the skin’s barrier, leading to inflammation and triggering or worsening symptoms.
- Skin Barrier Defects: People with eczema tend to have a compromised skin barrier, which makes it easier for irritants, allergens, and microbes to penetrate the skin and trigger reactions.
- Stress: Emotional stress and anxiety can weaken the immune system and trigger or exacerbate symptoms in some individuals.
Identifying and avoiding these triggers, along with proper skin care and management strategies, can help you better control your eczema and reduce the frequency and severity of flare-ups.
Diagnosis Process for Eczema

If you suspect that you have eczema, it is important to see a dermatologist or other healthcare provider for a proper diagnosis. Your healthcare provider will perform a physical exam and may also take a skin biopsy or patch test to help determine the type of dermatitis you have and its underlying cause.
Diagnosis is a multifaceted process that involves a combination of clinical observation, medical history assessment, and sometimes, additional tests. A dermatologist, a specialized doctor in skin health, is the most qualified professional to make an accurate diagnosis.
Clinical Observation

During a clinical examination, the dermatologist closely inspects the affected skin. They examine the pattern of redness, inflammation, and any visible changes. The dermatologist might ask about family history, previous skin conditions, and exposure to potential triggers.
Medical History Assessment
Understanding the patient’s medical history is crucial in determining whether the symptoms align with eczema. The dermatologist might inquire about allergies, dietary habits, exposure to irritants, and other relevant factors. This information helps rule out other skin conditions that might mimic eczema’s symptoms.
Allergy Skin Patch Testing
In some cases, patch testing might be recommended. This involves applying small amounts of various substances to the skin to identify potential allergens that could be triggering or exacerbating your symptoms. Patch testing is especially helpful when contact dermatitis caused by allergens or irritants, is suspected.
O
Skin Biopsy

While rare, a skin biopsy might be conducted to confirm the diagnosis. A small sample of the affected skin is examined under a microscope to determine the presence of specific changes indicative of eczema. Biopsies are generally reserved for cases where the diagnosis remains uncertain after clinical observation and other assessments.
Differential Diagnosis: Ruling Out Other Conditions

One of the challenges in eczema diagnosis is distinguishing it from other skin conditions with similar symptoms. Psoriasis, fungal infections, and allergic reactions can sometimes present symptoms resembling eczema. This is why seeking professional medical advice is crucial for accurate diagnosis and tailored treatment.
Common Eczema Treatment Options
There is no cure for eczema, but there are several treatments available to help manage the symptoms. The most common dermatitis treatment is topical creams and ointments, which can help soothe and moisturize the skin. In severe cases, oral medications or light therapy may also be recommended.
Antihistamines

Antihistamines are a type of medication commonly used to relieve symptoms associated with allergies, such as itching, sneezing, and runny nose. While antihistamines are not typically considered a primary treatment for eczema, they can still offer some benefits for individuals.
However, it’s important to note that antihistamines may not be the most effective or targeted treatment for eczema. They can provide temporary relief from itching, but they won’t address the underlying causes, or help repair the skin barrier.
Biologics: For Moderate to Severe Cases

Biologics are a class of medications that can be used to treat moderate to severe eczema that hasn’t responded well to other treatments. Biologics are a more recent addition to the treatment options for eczema and work by targeting specific components of the immune system that contribute to the condition.
These injectable medications are available by prescription under the name Dupixent® (dupilumab), and Adbry® (tralokinumab-ldrm).
Biologics have shown promising results for many individuals with severe symptoms, but they are not a first-line treatment due to their cost, potential side effects, and the need for medical supervision.
Oral Immunosuppressants
Oral immunosuppressants and Janus kinase (JAK) inhibitors are types of systemic medications used to treat moderate to severe eczema that haven’t responded well to other treatments. These medications target the immune system to reduce inflammation and control symptoms.
Pain Relievers, Like NSAIDs

Pain relievers, specifically nonsteroidal anti-inflammatory drugs (NSAIDs), can be used to help manage certain symptoms associated with eczema.
While pain relievers won’t directly treat the underlying causes, they can provide relief from the pain, discomfort, and inflammation that often accompany the condition.
Phototherapy Treatments

For cases that require more intensive treatment, phototherapy stands as a promising option. This treatment involves exposing the skin to controlled amounts of natural or artificial ultraviolet light. Phototherapy has shown remarkable success in reducing inflammation and alleviating symptoms, under the guidance of experienced medical professionals.
Topical Eczema Medications

When it comes to topical treatments, striking a balance between effective relief and safety is paramount. Corticosteroids are commonly prescribed to manage inflammation during flare-ups. However, our experts advise their cautious use under medical supervision due to potential side effects. Non-steroidal options like calcineurin inhibitors offer an alternative for sensitive areas such as the face.
OTC Hydrocortisone
Over-the-counter (OTC) hydrocortisone is a topical corticosteroid medication that can be used to help manage the symptoms of eczema. Hydrocortisone works by reducing inflammation and suppressing the immune response that contributes to these symptoms.
Prescription Topical Steroids
Prescription topical steroids belong to the corticosteroid family and are more potent than over-the-counter (OTC) hydrocortisone creams. They are typically prescribed by healthcare professionals to treat moderate to severe cases of eczema.
Natural Remedies for Eczema

Natural remedies for eczema have gained popularity due to their potential effectiveness and minimal side effects. These remedies often focus on moisturizing the skin, reducing inflammation, and promoting healing. Let’s explore some of the top natural remedies you can incorporate into your eczema management routine.
Aloe Vera Gel

Aloe vera gel is renowned for its healing properties. It contains antioxidants and compounds that can reduce redness and inflammation. Applying fresh aloe vera gel or a quality store-bought version can offer a cooling sensation and promote skin healing.
Coconut Oil

Coconut oil is a versatile remedy known for its moisturizing properties. Its rich fatty acids can help restore the skin’s natural barrier and lock in moisture. Applying coconut oil to affected areas can alleviate dryness and reduce itching.
Evening Primrose Oil
Evening primrose oil is rich in gamma-linolenic acid, which can help reduce inflammation. Consuming evening primrose oil supplements or applying the oil topically might aid in managing symptoms.
Oatmeal Baths

Oatmeal baths are a classic remedy for soothing dermatitis-prone skin. Oats contain compounds that can ease inflammation and itching. Adding colloidal oatmeal to your bath or making an oatmeal paste to apply directly to your skin can provide relief.
Tea Tree Oil

Tea tree oil possesses natural antiseptic and anti-inflammatory qualities. When diluted with carrier oil, it can be applied topically to help soothe irritated skin and prevent infection.
Sometimes, eczema can clear up without treatment, but this is not always the case. Discussing your treatment options with your doctor and finding the best combination that works for you is important.
Eczema Prevention Tips
Dealing with eczema can be challenging, but with the right strategies, you can significantly reduce the frequency and intensity of flare-ups. While there’s no one-size-fits-all solution, understanding effective prevention methods can make a world of difference in managing this condition and improving your quality of life.
Avoid Extreme Temperatures

Both cold and hot temperatures can trigger eczema flare-ups. Protect your skin from harsh weather conditions by wearing appropriate clothing and using humidifiers in dry environments to maintain optimal moisture levels.
Be Cautious with Allergens
Allergens can play a significant role in eczema flare-ups. Regularly clean your living space, vacuum carpets, and wash bedding to reduce allergen exposure. If you have pets, make sure to groom them frequently to minimize pet dander.
Choose the Right Clothing
The fabric you wear can impact your skin’s health. Opt for soft, breathable fabrics like cotton, which reduce friction and irritation. Avoid harsh materials like wool, as they can trigger itching and worsen symptoms.
Identify Triggers
Every individual’s eczema triggers can be different. Common triggers include certain foods, allergens, stress, and harsh skincare products. Keep a journal to track flare-ups and potential triggers, helping you identify patterns and make necessary lifestyle changes.
Keep Your Skin Moisturized

One of the key factors in preventing flare-ups is maintaining proper skin hydration. Regularly applying a gentle, fragrance-free moisturizer helps create a barrier that locks in moisture and prevents the skin from becoming dry and irritated.
Manage Stress Effectively
Stress is known to exacerbate eczema symptoms. Engage in relaxation techniques such as deep breathing, yoga, or meditation. Finding healthy ways to cope with stress can contribute significantly to preventing flare-ups.
Maintain a Balanced Diet

While there’s no specific “eczema diet,” consuming a balanced and nutrient-rich diet can support your skin’s health. Focus on foods rich in omega-3 fatty acids, antioxidants, and probiotics, as they can help reduce inflammation and boost your immune system.
Practice Good Hygiene

Maintaining good hygiene is crucial for eczema prevention. Take short showers using lukewarm water and a mild, fragrance-free cleanser. Afterward, gently pat your skin dry with a soft towel, ensuring you don’t rub or scrub your skin vigorously.
Protect Your Skin from Irritants

Certain household products and chemicals can trigger eczema symptoms. When using cleaning products or other potentially irritating substances, wear gloves to protect your hands and minimize contact with your skin.
Silicone may be to blame as well. New on the scene is the prevalence of silicone allergies. Silicone is used in many household products like gloves, bakeware, and even cosmetics.
Regularly Trim Nails
Long nails can inadvertently cause skin damage due to scratching, which worsens eczema symptoms. Keeping your nails short can help prevent accidental irritation and potential infections.
Seek Professional Advice

If your dermatitis is severe or difficult to manage, consult a dermatologist. They can provide personalized guidance and recommend treatments tailored to your specific condition.
Stay Consistent with Treatment
If your doctor has prescribed medication or topical treatments, be consistent in their use. These treatments can help manage symptoms and prevent flare-ups when used as directed.
Stay Hydrated

Drinking plenty of water is essential for overall skin health. Hydration from within helps maintain skin elasticity and reduces the likelihood of dryness and irritation that can trigger flare-ups.
Use Mild Skincare Products

Harsh soaps and skincare products with fragrances can strip your skin of its natural oils, leading to flare-ups. Opt for mild, hypoallergenic products that are specifically designed for sensitive skin.
A great brand to check out is Pure Haven. They specialize in personal care and home products that are completely safe, effective, non-toxic, and chemical-free.
What has been your experience?
Eczema is a chronic condition that can be frustrating and painful to manage.I am interested in hearing your story! Please send me an email: Chris@allergypreventions.com
Did you know? There are ways to Naturally Get Rid of Eczema Without Steroids.

