Having grappled with pollen allergies throughout my entire life, I find myself intimately familiar with the relentless onslaught of seasonal allergy symptoms that persist year-round. The perpetual battle against sneezing fits, itchy eyes, and nasal congestion has shaped my journey, instilling in me a deep understanding of the daily struggles faced by fellow pollen allergy sufferers.
Together, let’s unravel the intricacies of living with pollen allergies and discover a roadmap to a more comfortable and fulfilling life despite the persistent challenges that nature throws our way.

As an Amazon Associate, I may get compensation for qualifying purchases.
Table of Contents
Understanding Pollen Allergies
Pollen allergies, called hay fever or allergic rhinitis, manifest when the immune system excessively responds to pollen produced by trees, grasses, and weeds. Pollen, a fine powder discharged by plants as a component of their reproductive cycle, triggers these allergic reactions.
I understand pollen allergies very well, as my pollen allergy almost killed me. First, we need to get a better understanding of the three main types of pollen to blame for pollen allergies.
Types of Pollen
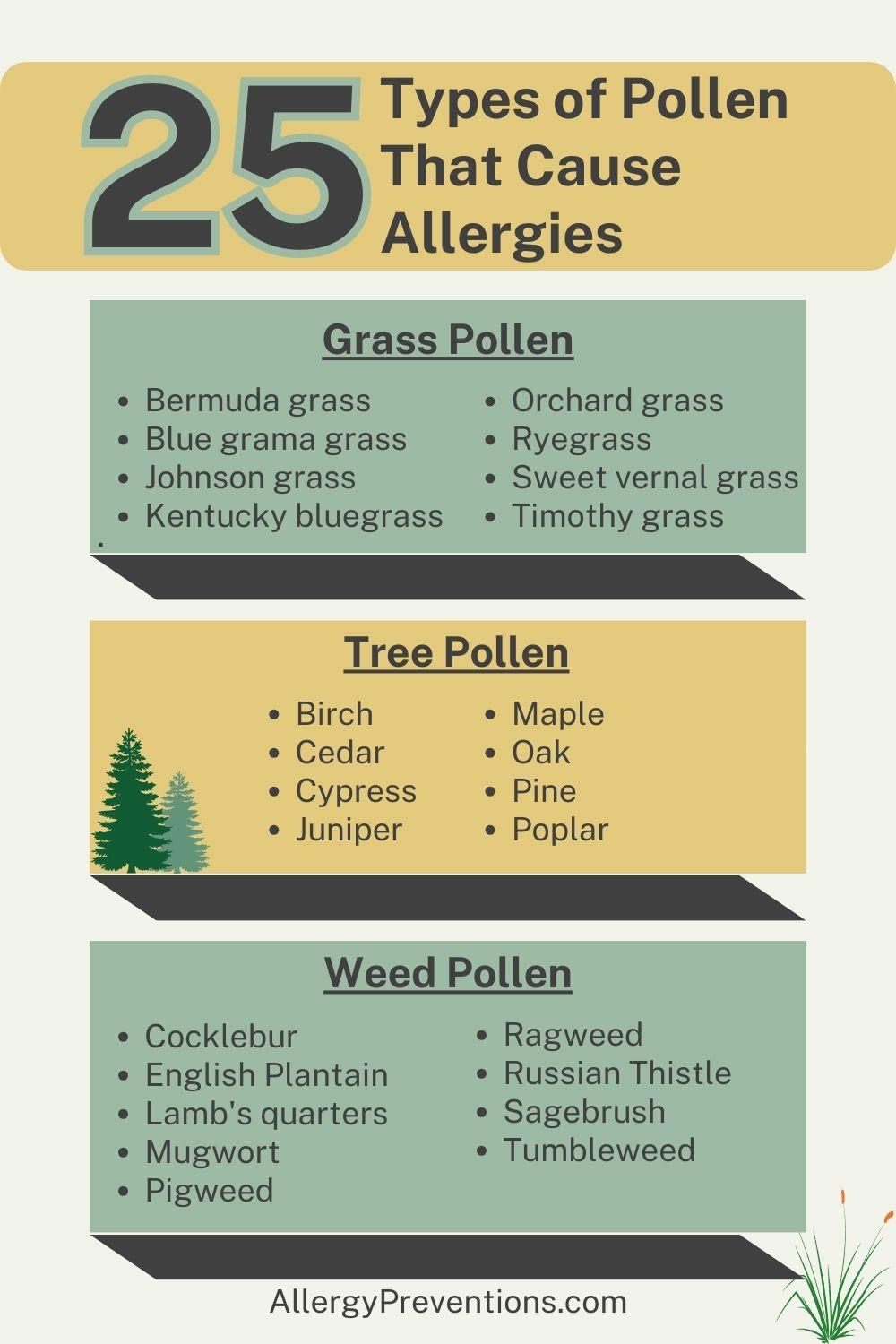
Pollen is a fine powder consisting of microscopic grains produced by the male reproductive parts of three main flowering plants. Pollen allergies can be triggered by various types of pollen from trees, grasses, and weeds. The main types of pollen are:
Grass Pollen
- Bermuda grass
- Blue grama grass
- Johnson grass
- Kentucky bluegrass
- Orchard grass
- Ryegrass
- Sweet vernal grass
- Timothy grass
Tree Pollen
- Birch
- Cedar
- Cypress
- Juniper
- Maple
- Oak
- Pine
- Poplar
Weed Pollen
- Cocklebur
- English Plantain
- Lamb’s quarters
- Mugwort
- Pigweed
- Ragweed
- Russian Thistle
- Sagebrush
- Tumbleweed
If you happen to be the “fortunate” individual dealing with allergies to all three types of pollen (like me) – trees, grasses, and weeds – it becomes crucial to remain vigilant about your activities and surroundings year-round.
Pollen Cross-reactivity & Food Allergies

Pollens from various plants contain proteins that share structural similarities, leading to the immune system recognizing them as alike. When an individual is allergic to one type of pollen, their immune system may react to similar proteins in other pollens, causing a cross-reaction.
For example, someone allergic to birch pollen might experience symptoms when exposed to certain fruits, vegetables, or nuts, like apples, carrots, or hazelnuts. This is due to the presence of proteins in these foods that resemble those found in birch pollen.
The immune system, sensitized to birch pollen, may mistakenly identify these proteins in food as a threat, triggering an allergic response.
Understanding cross-reactivity is important in managing allergies, as individuals with pollen allergies may need to be cautious about certain foods during peak pollen seasons.
Pollen Allergy Symptoms
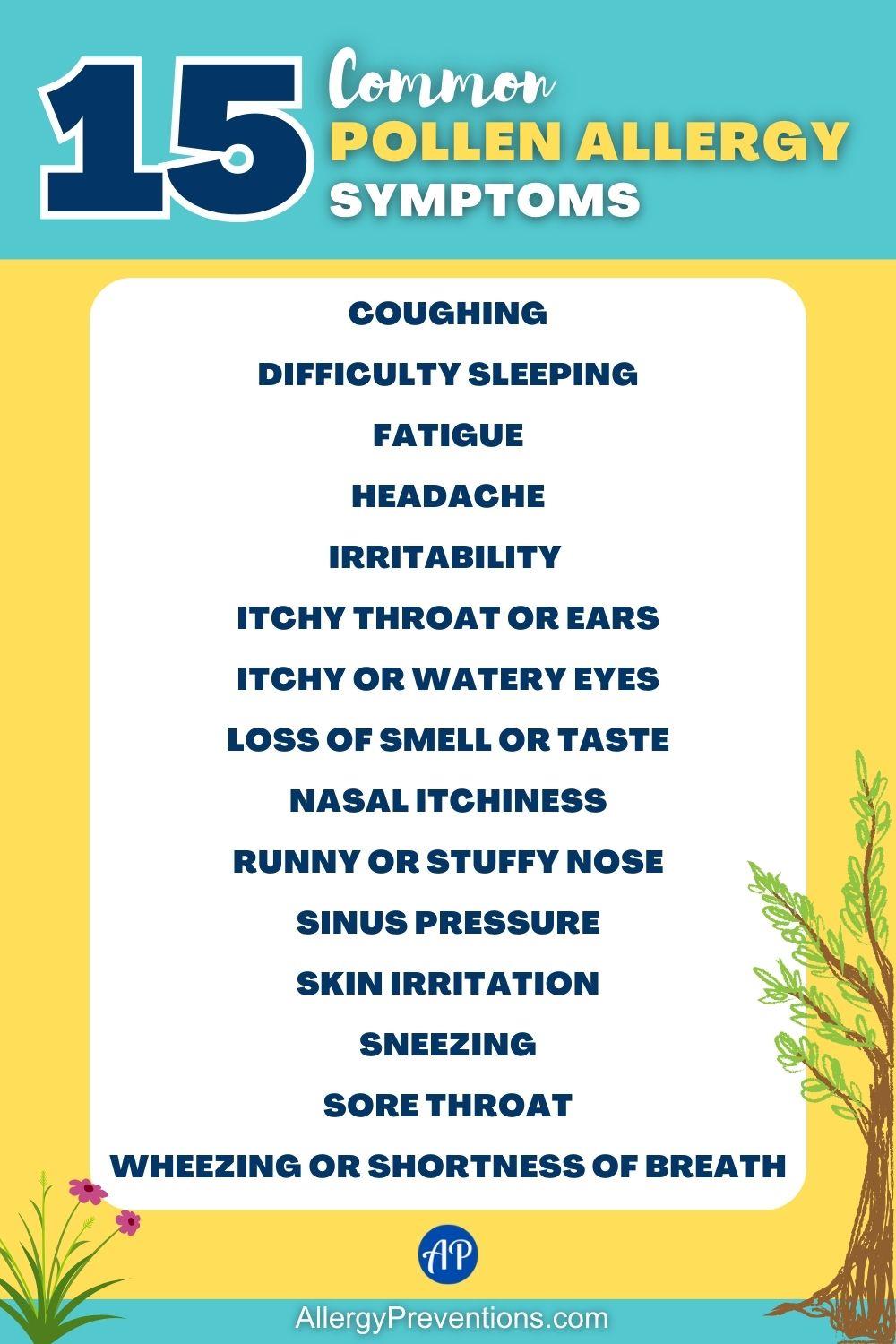
Pollen allergies can cause a variety of symptoms. The severity and combination of symptoms can vary among individuals. Here’s a detailed list of common symptoms associated with pollen allergies:
- Coughing: Persistent allergy-related coughing may be triggered by postnasal drip or throat irritation.
- Difficulty Sleeping: Allergy symptoms, especially nasal congestion, can interfere with sleep quality.
- Fatigue: Allergic reactions can lead to fatigue and a general feeling of being unwell.
- Headache: Some individuals may experience headaches as a result of nasal congestion and sinus pressure.
- Irritability: Discomfort and fatigue from allergies can contribute to irritability and mood changes.
- Itchy Throat or Ears: A scratchy or irritated sensation in the throat or ears can occur due to pollen exposure.
- Itchy or Watery Eyes: Irritation and discomfort in the eyes, often accompanied by redness and excessive tearing in one, or both eyes.
- Loss of Smell or Taste: In some cases, a temporary loss or alteration of the sense of smell or taste may occur.
- Nasal Itchiness: The nasal passages may feel itchy or irritated, prompting frequent rubbing or itching.
- Runny or Stuffy Nose: The nasal passages may become congested or produce excess mucus.
- Sinus Pressure: A feeling of pressure or fullness in the face, especially around the eyes and forehead.
- Skin Irritation: Allergic reactions to pollen can sometimes manifest as skin issues, such as hives or eczema.
- Sneezing: Frequent and uncontrollable sneezing is a common symptom of pollen allergies.
- Sore Throat: Postnasal drip can lead to a sore or scratchy throat.
- Wheezing or Shortness of Breath: Individuals with asthma or other respiratory conditions may experience worsened symptoms during the pollen season.
It’s important to consult with a healthcare professional if you suspect you have pollen allergies, as they can provide an accurate diagnosis and recommend appropriate treatment options, such as antihistamines, nasal corticosteroids, or allergy shots.
Diagnosing Pollen A Allergy

Pollen allergies are typically diagnosed through medical history, physical examination, and allergy testing. Here are the common diagnostic methods:
- Medical History: Your doctor will start by asking about your symptoms, their frequency, and any patterns you may have noticed. They may inquire about when your symptoms occur and whether there is a seasonal pattern, which can be indicative of pollen allergies.
- Physical Examination: A physical examination may be conducted to rule out other possible causes of your symptoms. For pollen allergies, the focus is often on the respiratory and nasal areas.
Pollen Allergy Testing

Pollen allergy testing is a diagnostic procedure designed to identify specific allergens that may be triggering allergic reactions in individuals. There are several methods commonly used for pollen allergy testing:
Nasal Smear (Cytology): This involves taking a sample from your nasal secretions to examine under a microscope for the presence of white blood cells associated with allergic reactions.
Skin Prick Test: Small amounts of allergens, including various pollens, are applied to your skin with a tiny needle. If you are allergic, you will develop a small raised bump at the test site.
Blood Test (Specific IgE Test): A blood sample is taken to measure the level of specific antibodies (immunoglobulin E or IgE) produced in response to allergens. Elevated IgE levels for specific pollens can indicate an allergy.
Once diagnosed, your healthcare provider will work with you to develop a management plan, which may include allergen avoidance strategies, and medications (antihistamines, decongestants, nasal corticosteroids).
In some cases, immunotherapy (allergy shots or sublingual tablets) may be recommended to desensitize your immune system to specific allergens, including pollen.
Pollen Allergy Breakdown by Season

The types of pollen released by plants vary with the seasons. While tree, grass, and weed pollen may be present throughout the year, specific seasons witness the peak prevalence of each type. Here is the pollen breakdown by season:
- Spring Allergies: Tree pollen dominates during spring, causing heightened allergic reactions for those with tree pollen allergies.
- Summer Allergies: Grass pollen is a primary culprit during the summer months.
- Fall Allergies: Weed pollen, particularly from ragweed, are the main triggers in the fall.
- Winter Allergies: Pollen from evergreen trees, or areas with extended growing seasons, may have elevated pollen levels during winter.
Protective Measures
To minimize exposure to pollen and alleviate allergic reactions, individuals can adopt various pollen protective measures, especially during peak pollen seasons. Here are some recommendations:
- Monitor Pollen Levels: Check daily pollen forecasts through an app to be aware of high pollen days, and adjust your schedule around peak pollen hours.
- Keep Windows Closed: Prevents pollen from entering your home.
- Use Air Purifiers: Air purifiers with HEPA filters reduce airborne pollen indoors.
- Limit Outdoor Activities: Reduce outdoor activities, especially in the early morning and late afternoon when pollen levels are often higher.
- Wear Sunglasses: Glasses can protect your eyes from a substantial amount of airborne pollen when outdoors.
- Change Clothes and Shower: Removes pollen from your body and hair.
- Keep Pets Clean: Wipe down pets to remove any pollen they may have picked up on their fur.
- Avoid Drying Clothes Outside: Avoid hanging laundry outside during peak pollen seasons, as pollen can stick to clothing.
- Use Allergy-Friendly Landscaping: Choose low-allergen plants for your garden and avoid planting high-pollen trees or flowers close to your home.
- Close Car Windows: Keep car windows closed during high pollen seasons and use air conditioning with a clean filter.
- Use Allergy-Proof Bedding: Use hypoallergenic pillowcases and mattress covers to reduce exposure to pollen while sleeping.
- Take Medications as Prescribed: If prescribed by your doctor, take allergy medications regularly to manage symptoms.
- Consider Immunotherapy: Discuss allergen immunotherapy options with your healthcare provider, such as allergy shots or sublingual tablets, which can help desensitize your immune system to specific allergens.
Medications for Pollen Allergies
There are various medications available to manage symptoms of pollen allergies. These medications aim to alleviate allergic reactions and improve the quality of life for individuals affected by pollen allergies. Some common types of medications include:
- Antihistamines: Over-the-counter antihistamines help alleviate symptoms by blocking histamine release, and reducing sneezing and nasal congestion.
- Decongestants: Oral or nasal decongestants provide temporary relief from congestion but should be used cautiously due to potential side effects.
- Eye drops: Over-the-counter allergy eye drops help relieve itchy, red, and watery eyes by leveraging their antihistamine properties. These eye drops also flush the eyes and reduce irritation.
- Nasal sprays: Corticosteroid nasal sprays mitigate inflammation and offer relief from nasal symptoms. Regular use can prevent symptoms from worsening.
- Prescription medications: Prescription-strength antihistamines, corticosteroids, and eye drops are available through your physician.
Natural Remedies
Natural remedies for pollen allergies include consuming local honey to build tolerance, incorporating quercetin-rich foods like apples and berries for their natural antihistamine properties, and trying nettle leaf supplements or tea for their anti-inflammatory effects.
Check out the 15 Natural Pollen Allergy Remedies article to find more ways to ease your symptoms.
However, individual responses vary, and for severe allergies or persistent symptoms, consulting with a healthcare professional is recommended for personalized advice and potential treatment options.
Conclusion
Living with pollen allergies requires proactive management and adaptation. By understanding individual triggers, implementing preventive measures, and exploring various treatment options, you can navigate the seasons with greater ease.
What is your next move? If you have not done so already, I recommend getting diagnosed first, and also consider getting a HEPA filter for your home.

I have a full review of our Winix 5500-2 HEPA filter, which we have been sporting since 2017, check it out. Or if you want to get straight to the price and stats, check it out on Amazon. We love ours, and it makes our home pollen-free all year.
