Spongiotic dermatitis is a common condition characterized by redness, itching, swelling, and inflammation of the skin. The word “Spongiotic” literally means excess fluid. This article aims to provide an in-depth understanding of spongiotic dermatitis, including its causes, symptoms, treatment, and prevention options.

As an Amazon Associate, I may get compensation from qualifying purchases.
Table of Contents
What is Spongiotic Dermatitis?

Spongiotic dermatitis (SD), is a blanket term for a type of skin inflammation characterized by redness, itching, and sometimes the formation of tiny blisters. It is often associated with allergies, irritants, or underlying skin conditions. Spongiotic dermatitis can affect people of all ages, from infants to the elderly, and it can occur on any part of the body.
An easy way for me to remember the term is that Spongiotic looks like it has the word “sponge” in it, which can have an excess of fluid.
Is spongiotic dermatitis curable?
Spongiotic dermatitis is not considered curable, but it is a manageable condition. With proper treatment, lifestyle adjustments, and ongoing care from a healthcare professional, individuals with spongiotic dermatitis can lead healthy and comfortable lives.
Medical research continues to advance, and new treatments are being developed. While spongiotic dermatitis may not be curable at the moment, future breakthroughs could offer additional options for managing the condition.
Causes of Spongiotic Dermatitis
The root cause of spongiotic dermatitis is not known and may vary from person to person. Scientists believe that spongiotic dermatitis most likely is caused by genetics, existing health conditions, or environmental factors.
Triggers
Spongiotic dermatitis can be triggered by many different factors, some of which you may be able to control. It’s important to note that triggers may be different for you compared to others. Identifying your specific triggers may require careful observation and consultation with a healthcare professional or dermatologist.
Allergies

When an allergen comes into contact with the skin, the immune system reacts abnormally, causing an immune response. This response leads to the release of chemicals that cause inflammation in the skin, potentially resulting in spongiotic dermatitis. Here are a few allergy triggers:
- Dust mites
- Food allergies
- Fragrances
- Latex
- Makeup
- Metals (nickel, copper, cobalt)
- Molds
- Pet dander
- Pollen
Environment

Weather can have a significant impact on spongiotic dermatitis and can act as a trigger for flare-ups in some individuals. Here’s how weather conditions can contribute to the development or worsening of spongiotic dermatitis:
- Dry air: Low humidity levels can cause the skin to become dry and lose moisture. This can lead to increased skin sensitivity and irritation, making it more prone to developing spongiotic dermatitis.
- Cold weather: Cold temperatures can exacerbate spongiotic dermatitis symptoms. Cold air can strip the skin of its natural oils, leading to dryness and increased itchiness. Additionally, the use of indoor heating systems during colder months can further dry out the air, aggravating the condition.
- Hot and humid weather: While dry weather can be problematic, high humidity levels can also trigger spongiotic dermatitis for some individuals. Excessive sweating caused by hot and humid conditions can lead to increased skin irritation and itchiness.
- Sun exposure: Ultraviolet (UV) radiation from the sun can aggravate spongiotic dermatitis symptoms. Sunburn can further damage the skin barrier, leading to increased sensitivity and inflammation.
High Histamine Foods

High-histamine foods can potentially trigger spongiotic dermatitis in certain individuals. When high-histamine foods are consumed, they can further contribute to this histamine imbalance in susceptible individuals.
These foods contain varying levels of histamine or can trigger the release of histamine in the body. When histamine levels increase, it can lead to an exaggerated immune response, causing or exacerbating spongiotic dermatitis symptoms.
Infections

Infections are one of the most common triggers for this condition, as they can cause the immune system to go into overdrive. Once an infection has resolved, the symptoms of spongiotic dermatitis will typically resolve on their own. However, in some cases, the condition may recur or become chronic.
Medications

Medications that can trigger spongiotic dermatitis include topical steroids, antimalarials, nonsteroidal anti-inflammatory drugs (NSAIDs), and immunosuppressants. When these medications are used, they can cause the walls of the skin cells to weaken, allowing fluid to leak out.
In addition, these medications can inhibit the production of substances that help to keep the skin moist and supple. As a result, the skin becomes dry, cracked, and inflamed. In severe cases, spongiotic dermatitis can lead to blistering and ulceration.
Skin Irritants & Chemicals

When our skin comes into direct contact with skin irritants or chemicals, such as certain cleaning agents, solvents, or even soaps, it can lead to irritation. These irritants can disrupt the skin’s natural barrier function. Here is a list of potential products that may be triggering your spongiotic dermatitis:
- Body wash
- Conditioner
- Fabric softener
- Face wash
- Hand soap
- Laundry detergent
- Shampoo
- Synthetic material (silicone)
Chemicals to Avoid

To avoid skin irritation, there are chemicals found in household products like soaps, makeup, and baby products. Here is a list of the most common chemicals found in household products:
- Cocamidopropyl betaine
- Formaldehyde
- Fragrances
- Isothiazolinone
- Parabens
- Paraphenylenediamine
- Phthalates
- Sodium lauryl sulfate (SLS)
- Sodium laureth sulfate (SLES)
Stress

When a person is under a lot of stress, their immune system can become weakened, making them more susceptible to skin problems. In addition, stress can also cause hormonal changes that can further contribute to skin inflammation. As a result, managing stress levels is often an important part of treating and preventing spongiotic dermatitis.
What does spongiotic dermatitis look like?
Spongiotic dermatitis tends to look like dry, red, swollen, blistering skin. Here is a list of the possible visual characteristics:
- Blisters/fluid-filled bubbles
- Dry skin patches
- Oozing
- Redness
- Skin scaling or flaking
- Swelling
- Watery discharge/weeping
Picture of Spongiotic Dermatitis on Fingers
This image of spongiotic dermatitis shows multiple blisters containing fluid on the hands. Although the cause of these blisters was not disclosed, it does seem like the cause may have been contact dermatitis.

Spongiotic Dermatitis on Forearm
This image shows us a more rash-like case of spongiotic dermatitis on the forearm. You can see some scaling, flaking, and blistering on the skin.

Blistering Spongiotic Dermatitis
This picture shows a side angle of a SD blister that has spread from the palm, down the side of the pinky. Notice there is a slight cut on the blister, broken skin can make you more prone to infections.

Spongiotic Dermatitis Symptoms

The symptoms of spongiotic dermatitis can vary from person to person. Symptoms are influenced by how you acquired dermatitis (immune, contact, infection, allergy). Here is a list of the most common symptoms associated with spongiotic dermatitis:
- Blisters
- Dry skin
- Flaking skin
- Itchy skin
- Pain (especially if the skin is broken or blistering)
- Rash
- Skin hardening
- Skin sensitivity
- Swelling of the skin
Risk Factors
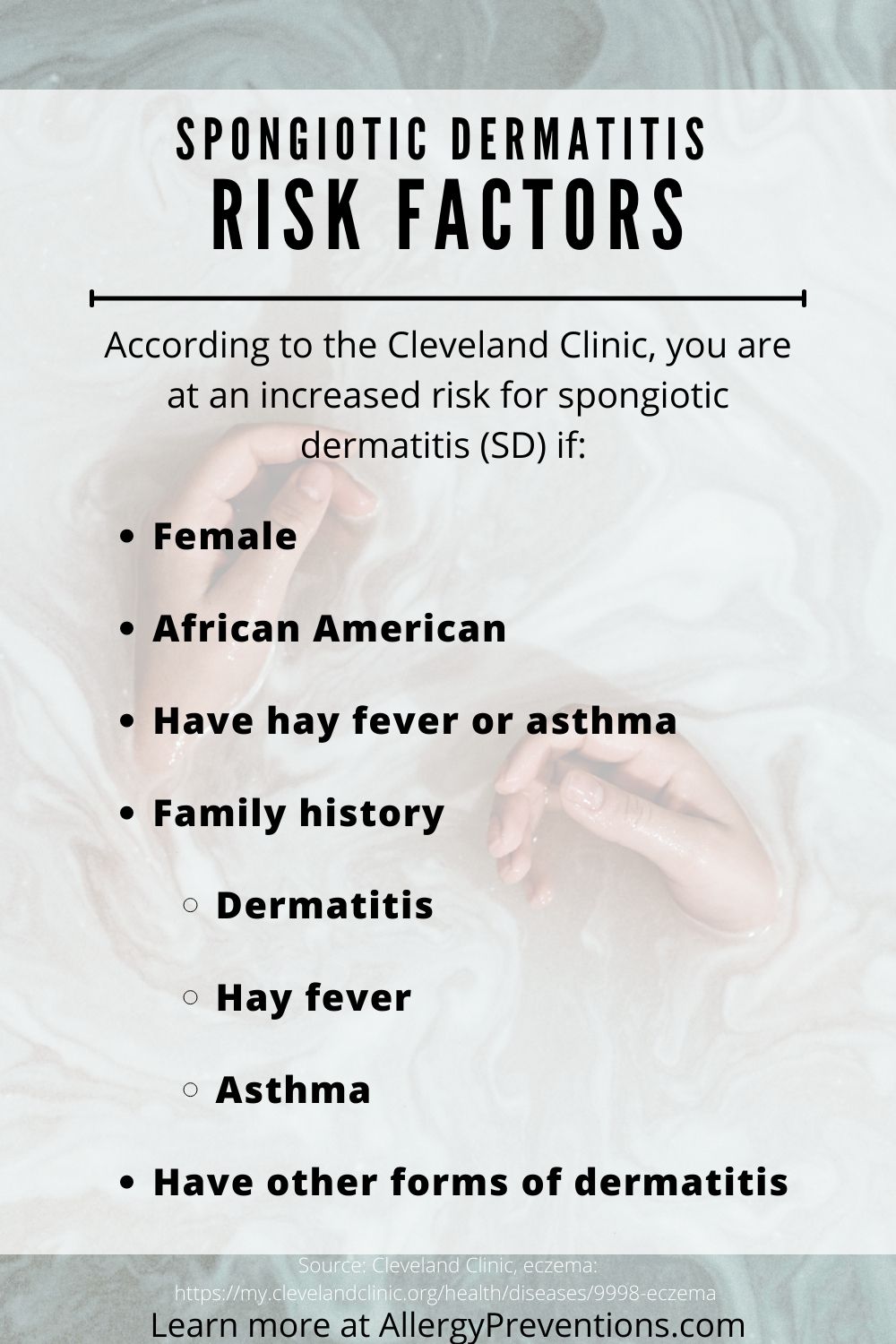
There are factors that may put you at an increased risk of having spongiotic dermatitis. Knowing the risk factors may help you and your medical provider in making a proper diagnosis. Here are some possible risk factors:
- African American
- Asthma
- Family history
- Female
- Hay fever
- Other forms of dermatitis
Diagnosis

According to the Cambridge University Press, spongiotic dermatitis is diagnosed as follows. First, SD is excess fluid (edema) under the skin, so your doctor may diagnose simply by your symptoms, health history, and how your skin looks. To get a true diagnosis of SD a skin biopsy is usually performed. The biopsy is sent to a pathologist to be examined under a microscope.
The pathologist will be able to determine what type of skin disorder is present and its severity. SD can be diagnosed into subclasses of acute, subacute, and chronic.
Acute: Short-term condition with a sudden onset, and may or may not resolve on its own.
Subacute: A condition that is not acute, but not yet chronic.
Chronic: Long-lasting condition that doesn’t go away, or keeps coming back.
The results from the biopsy will be documented and sent to your provider. A follow-up appointment is usually required to go through the results as well as discuss any potential treatment plans.
Outlook

The outlook of SD depends on the cause, severity, and whether the condition is considered acute, subacute, or chronic. Overall, the outlook is good with most cases being manageable. Of course, there are cases where you may have a bad flare-up which can lead to other complications including infections.
Complications
Complications may arise when managing spongiotic dermatitis, here are some complications you should be aware of. Many times the cause of complications is due to symptoms that are not well managed or continue to get worse regardless of proper treatment and prevention techniques.
Broken skin

Scratching, trauma, and swelling can lead to the skin breaking open. When the skin is broken, you may notice bleeding or weeping of liquid from your skin. Broken skin can cause complications by potentially limiting your range of motion (bandages, scabs, etc.) or by making you vulnerable to infections.
Infections
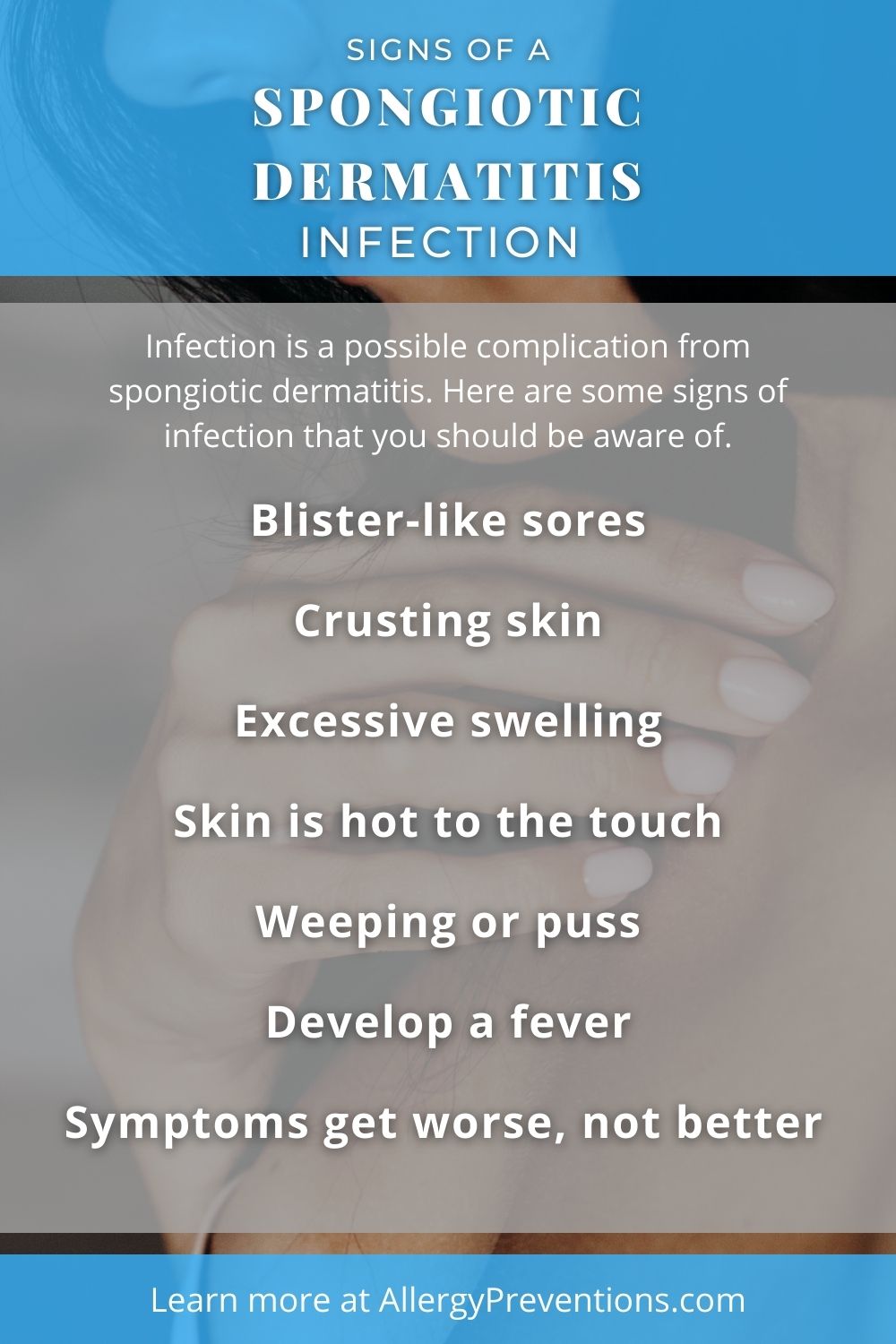
Infection is a possible complication of spongiotic dermatitis. Here are some signs of infection that you should be aware of:
- Blister-like sores
- Crusting skin
- Excessive swelling
- Fever
- Skin is hot to the touch
- Symptoms get worse, not better
- Weeping or puss
Infections are a condition that needs treatment. Seek medical assistance right away if you suspect an infection. Keep in mind this is not an all-inclusive list and you may experience different symptoms. When in doubt, see a medical professional.
Spongiotic Dermatitis Treatment

The good news is there are treatment options for spongiotic dermatitis symptoms. Treatment options are something you should be discussing with your doctor. Ultimately, this is an inflammation of your skin, so knowing the cause can be great information to have when starting a treatment plan.
For example, if the known cause of spongiotic dermatitis is allergies, avoiding those allergens or taking an antihistamine (treatment) can help with removing the symptoms.
A medical provider may suggest one of these treatment options, after this list of options you will find more details for each one below.
Antihistamines

Antihistamines work by lowering the amount of histamine in your body. Histamine is your body’s allergic response to something. If your dermatitis is caused by an allergic reaction, an allergy medication could help relieve your symptoms.
Prescription Medication

The prescription medicine world has an overwhelming amount of choices when treating SD. According to Drugs.com, there are 161 different medications that can be used for treating spongiotic dermatitis. Here are the categories of drug treatments that you can discuss with your doctor:
- Anorectal preparations
- Antihistamines, topical
- Anti-infectives, topical
- Emollients, topical
- Glucocorticoids
- Miscellaneous topical agents
- Rubefacients, topical
- Steroids, Topical
- Topical steroids with anti-infectives
Rethink your Shower

Showering or bathing can be relaxing, but if you suffer from spongiotic dermatitis, you may dread rinsing. Here are some pointers to keep your skin calm and potentially improve your symptoms:
- Avoid hot showers, and turn down the temperature a bit
- Make it a quick shower, under 10 minutes is ideal
- Pat your skin dry, don’t drag the towel across your skin
- Immediately apply your favorite hypoallergenic moisturizer
Topical Steroids

Topical steroids do really well at calming down the skin and easing inflammation. They are also good at stopping the itch while also providing some moisture to your mad skin. The strongest over-the-counter topical steroid is Cortizone 10® which contains 1% hydrocortisone. If you need a stronger topical steroid you will need a prescription.
Use a Moisturizer

Not all spongiotic dermatitis moisturizers are created equally. Some are light, and water-based, while others are thick, long-lasting, and oil-based. You will want to explore the moisturizers that work best for you.
Generally speaking, you should look for a moisturizer that does not have a laundry list of ingredients or that contain fragrance.
Creams
Creams usually contain a mix of oil-based moisturizers and a mix of water-based moisturizers. Keeping your skin moist may help in relieving itching, and dry flaky skin.
Lotions
Lotions are mostly water-based and provide a short-term moisture fix for your skin. If you need a lightweight moisturizer that isn’t greasy and you are able to apply it multiple times a day, lotion may be the best option for you.
Ointments
Ointments are the thickest and oil-based (usually petroleum jelly) but they provide the longest-lasting moisture. They are greasy, but they work! My recommendation would be to reserve using ointments for bad flare-ups, or as a treatment that you apply to your skin at night.
Prevention of Spongiotic Dermatitis
Preventing flare-ups to limit symptoms is a great approach when managing SD. The first step you should take is to know your triggers and avoid those triggers if possible. Above all, if it is not possible to avoid your triggers there are still some things you can do to hopefully make life a bit easier.
Apply moisturizer

When managing SD, moisturizers are going to become your best friend. The goal is to keep you and your skin happy and healthy. Healthy skin leads to fewer flare-ups and more mild symptoms. Therefore, when you choose a spongiotic dermatitis moisturizer, the more natural and fewer additives the better. For example, moisturizers with fragrances are a big “no-no”. Fragrances smell nice, but they tend to be major skin irritants.
Lower the Shower Temperature

Interestingly, our skin is sensitive to extreme temperatures, both hot and cold. When you have SD or any other skin condition, this sensitivity is amplified. To prevent flare-ups, lower the shower temperature, especially if you usually have it hotter than the surface of the sun (ladies).
Additionally, professionals recommend limiting the amount of time in the shower and to apply moisturizer within the first two minutes of getting out. Applying moisturizer right away helps your skin lock in moisture.
Ditch Harsh Skin Products

There are so many harsh products that we expose our skin to every day, and we might not even be aware! If you haven’t heard of the Environmental Working Group (EWG), you have to check it out. They have health ratings on many daily-use products.
Our family was shocked at how many “F” graded products we were using.
We have now switched to healthier choices with better ratings. Here are some products that I recommend you look into and replace if they have harmful ingredients:
- Bar soap
- Body wash
- Conditioner
- Cosmetics
- Dish soap
- Dryer sheets
- Fabric softener
- Face wash
- Handsoap
- Laundry detergent
- Lotion
- Shampoo
- Shaving cream
- Sunscreen
In my household, the worst products we were using were laundry detergent and household cleaners. Because of this, we have since switched to hypoallergenic soap products and we replaced ALL our household cleaners with Force of Nature Cleaner.
FAQs
We have made it to the frequently asked spongiotic dermatitis questions, which are ACTUAL FAQs from readers like you.
Is there a cure for spongiotic dermatitis?
No. There is no cure for SD, but knowing your triggers to avoid flare-ups can keep symptoms at bay.
Does spongiotic dermatitis go away?
Maybe. Spongiotic dermatitis can be caused by many factors including physical contact, and medications. Knowing the true cause of your SD will give you a better idea of whether your condition is acute or chronic.
Does spongiotic dermatitis spread?
Yes. Spongiotic dermatitis can spread on your skin, but it cannot be spread from person to person.
Is spongiotic dermatitis cancer?
No. Spongiotic dermatitis is a term to describe skin inflammation with fluid buildup under the skin.
Is spongiotic dermatitis contagious?
No. SD is not contagious and cannot be spread from person to person.
Is psoriasis spongiotic dermatitis?
No, these are two different conditions. Although the symptoms of spongiotic dermatitis (fluid in the skin cells) are seen in the early stages of psoriasis.
What is the most common cause of spongiotic dermatitis?
Atopic dermatitis. Atopic dermatitis is the most common type of dermatitis that presents spongiotic symptoms.
Is spongiotic dermatitis an autoimmune disease?
Yes. The major cause of SD is an inflammatory autoimmune skin disease.
What is spongiosis?
Presence of intercellular edema (fluid) in the skin. NIH.gov
Should I put moisturizer on dermatitis?
Yes. Dermatitis is an inflammation of the skin, and if your skin is dry, patchy, or itchy, unscented moisturizers can help calm the skin.
Can stress cause spongiotic dermatitis?
Yes. When we are stressed or anxious our body produces the stress hormone cortisol. This hormone can slow the healing process in the body and put your body at risk for an inflammatory response in the form of dermatitis.
What is the ICD 10 code for spongiotic dermatitis with eosinophils?
L98, Other disorders of skin and subcutaneous tissues, not elsewhere classified. or L30.9, Dermatitis unspecified
Final Thoughts
That is a deep dive into spongiotic dermatitis! I hope you have picked up some helpful information. The biggest takeaways are to get with your doctor, find a good moisturizer, and investigate your household products for harmful ingredients.
Don’t forget to check out:
10 Best Spongiotic Dermatitis Moisturizers
Spongiotic Dermatitis Foods to Avoid
Thank you for stopping by. Do you have any “infrequently” asked questions or an SD story you would like to share? Send me an email at: chris@allergypreventions.com
